The use of omni abutments on the aesthetic zone
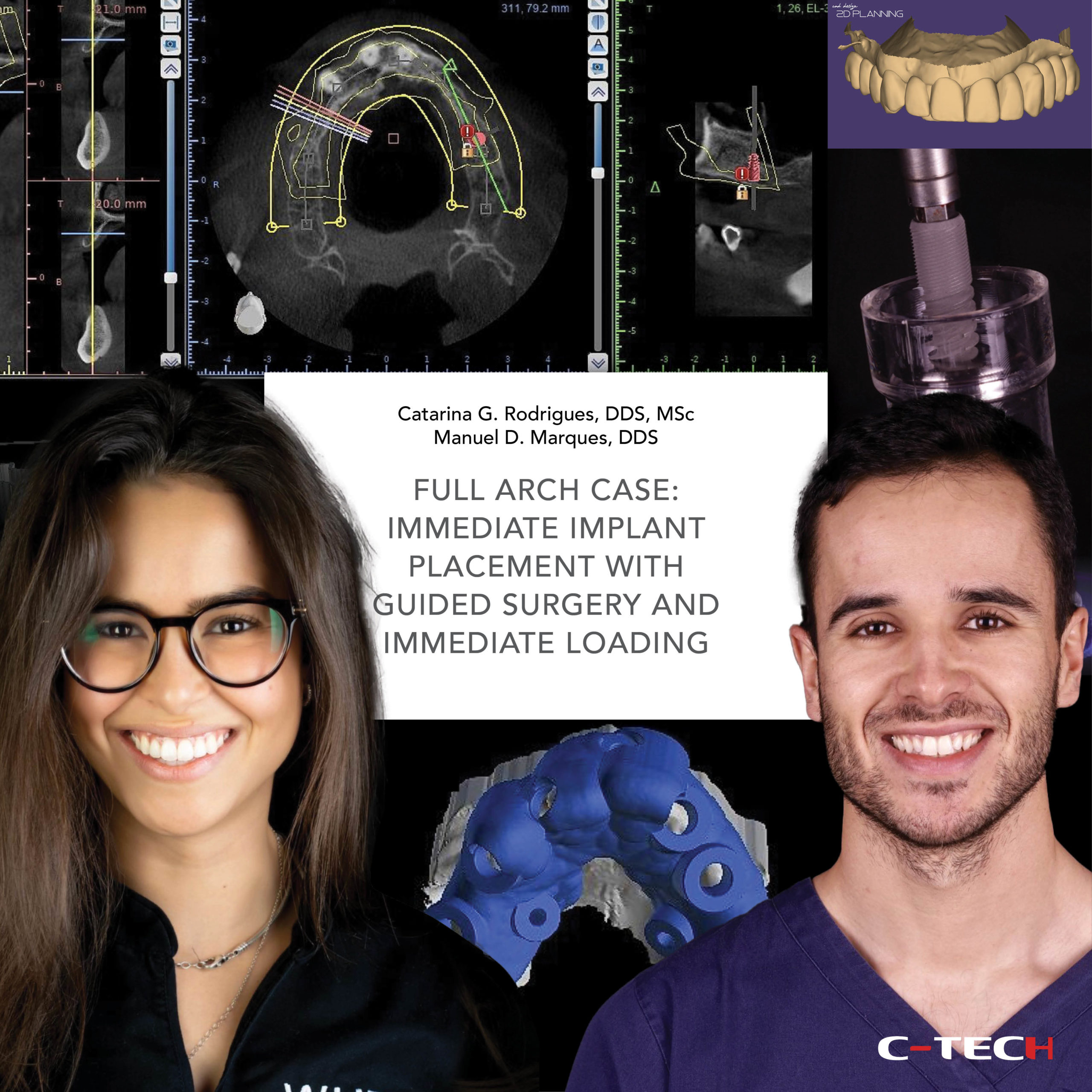
Dr. Catarina G. Rodrigues, DDS, MSc – Dr. Manuel D. Marques, DDS
A 65-year-old woman presented to a private practice with the main complaint being old dental treatments that were failing and poor aesthetics. The extra-oral pictures revealed a non-harmonious smile and severe upper midline deviation. The intra-oral and radiographic evaluation revealed bad marginal adaptation and fractured crowns, gingival recessions, presence of deep bite, extensively restored anterior teeth and a congenitally missing upper lateral incisor (Fig.1-3).
When doing the smile analysis it appeared that the previous doctor of the patient tried to transform the right canine into a lateral incisor with a ceramic crown, however the result was not aesthetically pleasant. Also, we figured that tooth proportions, general shape and colour were not correct. Finally, the position of the gingival margins was not harmonious. All the previously described situations combined were creating a dramatic aesthetic problem (Fig.4). In this case, especially because of the missing lateral incisor, a careful planning was of great importance for the final aesthetic outcome.
Following a comprehensive diagnosis, we concluded that the upper incisors were already very fragile, with history of multiple restorative and endodontic treatments and with a very questionable prognosis; that is why we finally decided to extract and replace it with dental implants. Regarding the implants that the patient already had on the second quadrant, it was decided to maintain them, as they did not present any sign of infection. Only the crowns over the implants were planned to be replaced.

For the anterior bridge, we decided to use OMNI abutments as the intermediate prosthetic component due to its smaller width, compared with the MUA. For this specific case, the plan was to do an implant supported restoration without pink component, which means the restoration should emerge directly through the gum, simulating the natural dentition. For these kinds of cases is very important to choose a prosthetic component that most closely resembles the dimensions of natural teeth (Fig.5,6).
To perform the pre-surgical planning of the case, initial records of the patient were obtained: intra and extra-oral photographs, digital impressions, and CBCT (Fig.7). A 2D facially driven digital smile design was made to aid in the planning of the position and dimension of the teeth for the future interim prosthesis. In the 2D smile simulation, by correcting tooth proportions and dimensions, and, also, the position of the midline, it was possible to generate the space for the right lateral incisor that was missing (Fig.8).
The 2D smile simulation was sent to the lab and used to create a 3D diagnostic wax-up. The mock-up was then tried on the patient’s mouth. The patient was very happy with the new appearance of the smile, especially regarding the right lateral incisor that she never had before.
The mock-up was approved and used to plan the position of the implants. The planning of the implants based on the desired final position of the teeth is a key factor of success in implant dentistry (Fig.9).

The STL file of the mock-up was superimposed with the preoperative intra-oral scan and CBCT to digitally plan the implant surgery. Once the future implant positions were defined, they were translated into the design of the surgical template. The size of the prosthetic abutments was also planned in the same software (Fig.10-14).
The provisional restoration was also fabricated previously to the surgery. In addition, a guide to aid on the proper positioning and stabilization of the provisional restoration, during the immediate loading, was fabricated (Fig.15-17).
Following local anesthesia, a sharp dissection of the supracrestal fibers with a micro scalpel blade was performed and the anterior teeth were removed carefully with extraction forceps in order to preserve, as much as possible, the soft and hard tissues. The socket was thoroughly debrided with a surgical excavator and rinsed with saline. The integrity of the buccal wall was verified (Fig.18).
Then, the surgical guide was placed and checked for its fit and stability. All implant sites were prepared through the guide (Fig. 19).

A 3.8×13 mm implant was placed at the 1.4 site. After that, an anchor stent was placed on the implant, through the guide, to increase its stability and precision (Fig. 20-21).
Finally, two 3.8×13 mm implants were placed at 1.1 and 2.2 sites (Fig. 22-25). The occlusal control picture revealed an adequate 3D positioning of the implants (Fig. 26). After implant placement, the prosthetic components, in this case the OMNI abutments, were placed (Fig. 27).

Then, in order to obtain the immediate provisional restoration, temporary titanium abutments were attached to the OMNI abutments. The ideal position of the interim prosthesis was obtained using a proper guide. This guide also helped with stabilization of the future teeth. Then, the provisional teeth were connected to the temporary abutments using tooth colour acrylic resin. To compensate for the changes in the soft tissue contour that spontaneously occur following a tooth extraction, which can have a negative impact on the health of peri-implant tissues, and compromise the final aesthetic result, a simultaneous soft tissue augmentation, at the time of dental implant placement, using a connective tissue graft, was performed.
The post-operative panoramic x-ray revealed ideal implant position and proper fit of the immediate restoration (Fig 28-32). The control appointment, 1 week after the surgery, revealed a good healing, and also, a very noticeable aesthetic improvement (Fig.33,34).
Four months after the surgery we proceed with the final impressions. A complete digital workflow was followed (Fig 33-36).

The final restorations were produced using CAD-CAM technology (Fig.37-39).
We finally delivered a bridge over teeth from 1.7 to 1.5, a crown over implant on 1.4, single crowns over teeth on 1.3 and 2.3, a bridge over implants from 1.2 to 2.2, and also, a bridge over implants from 2.4 to 2.6 (Fig.40-45).
The final intra and extra-oral photographs revealed that we managed to correct the position of the upper midline, to improve the shape and proportions of the teeth, to correct the deep bite and the position of the gingival margins, and to create space for the right lateral incisor that was missing, obtaining a very harmonious and aesthetically pleasant smile (Fig.46-51).

The final panoramic x-ray revealed proper adaptation of the final restorations (Fig. 52).

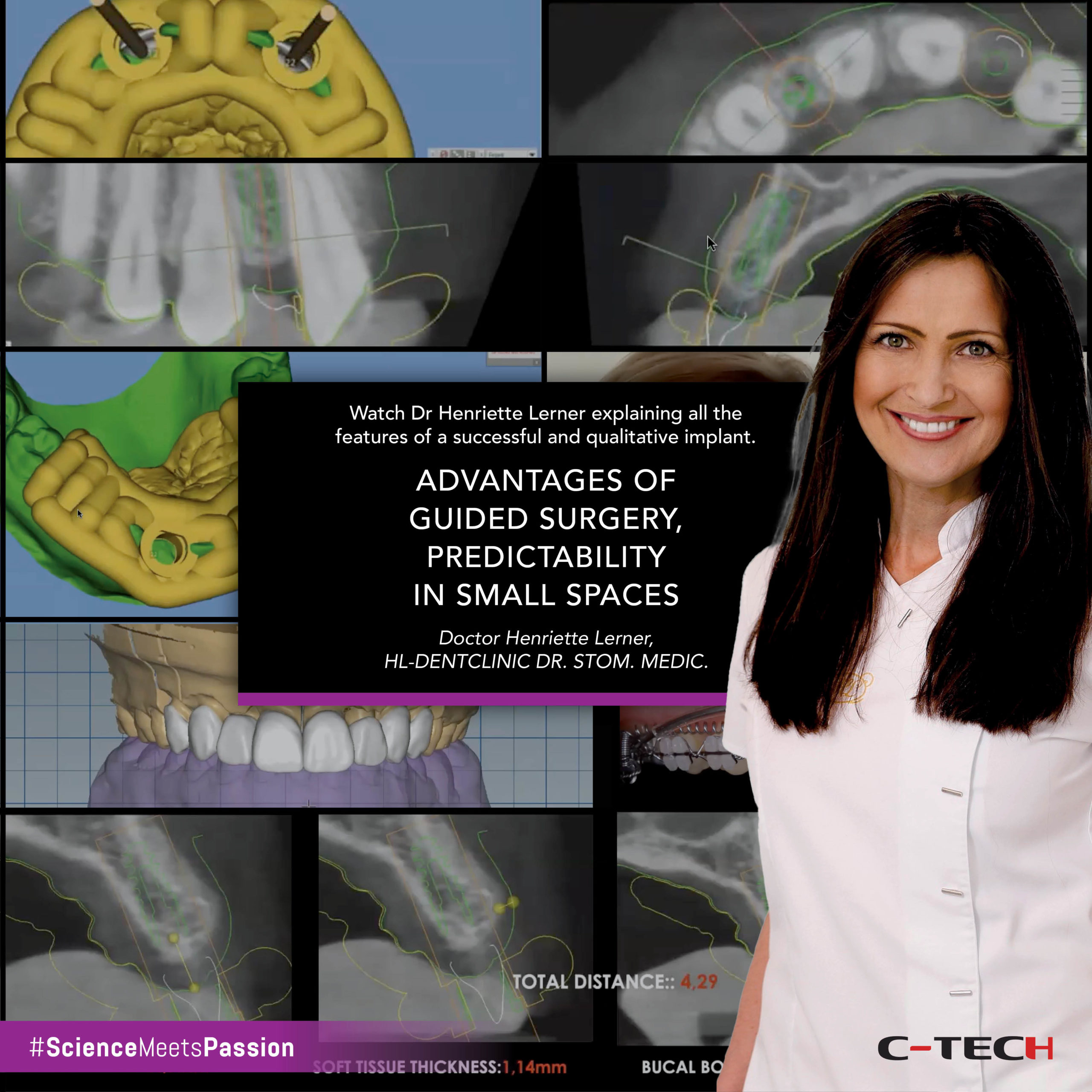
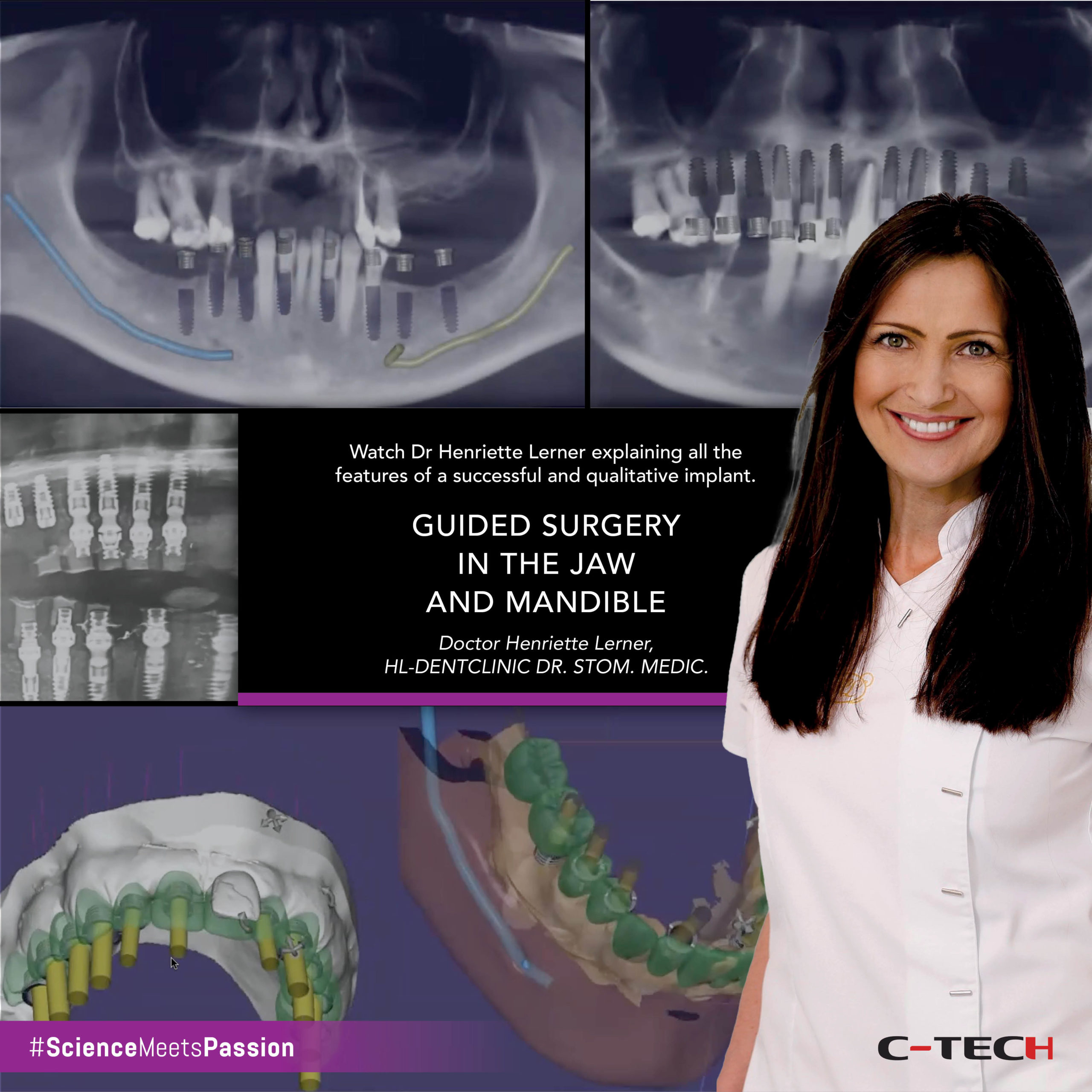
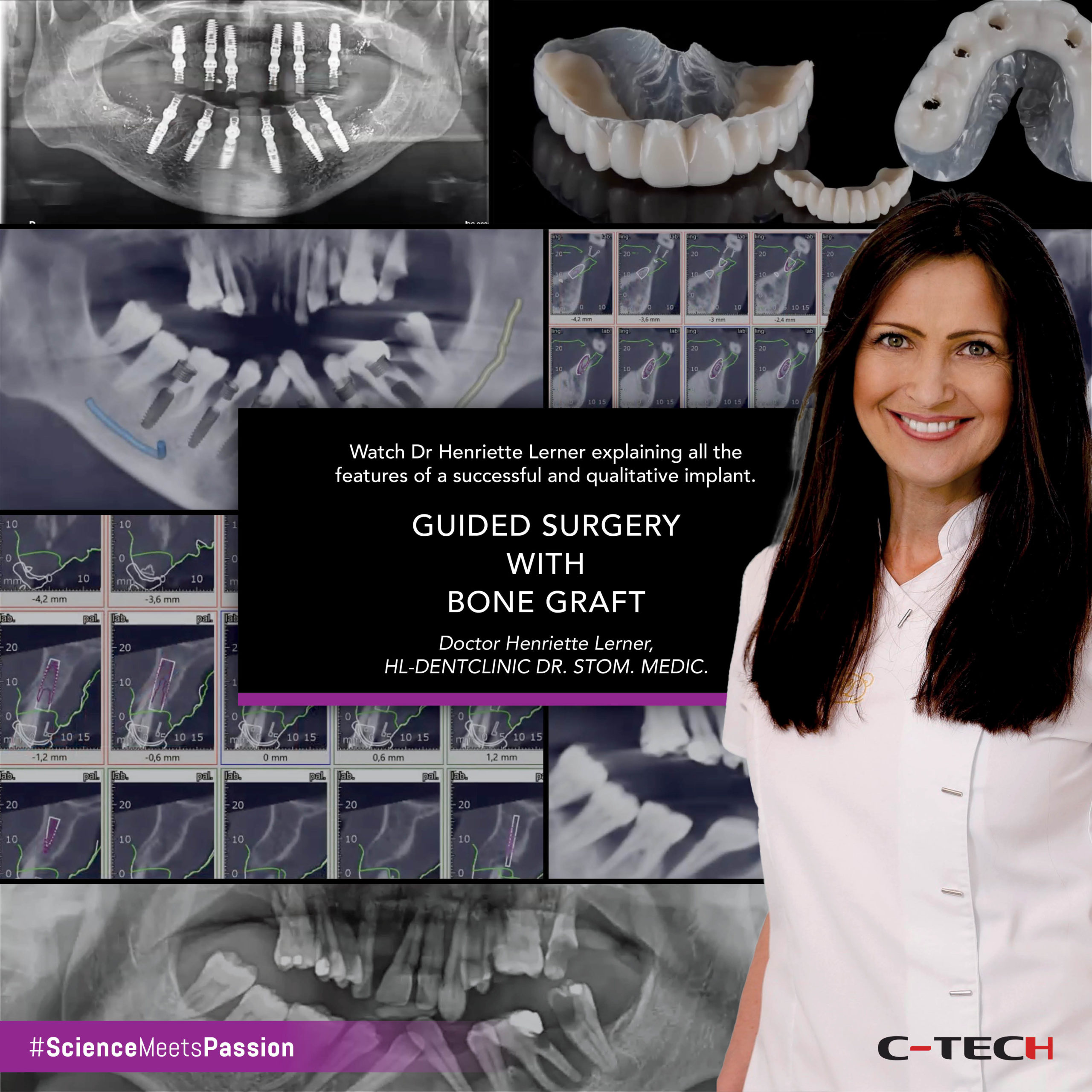
Webinar | OMNI AESTHETIC SOLUTIONS: from single units to full arch
Catarina G. Rodrigues, DDS, MSc • Manuel D. Marques, DDS
This webinar introduces the OMNI abutment by C-Tech, a versatile prosthetic component designed to achieve excellent aesthetic results across various dental cases, from single units to full arches. The presentation begins with a complex full-mouth case demonstrating the OMNI abutment’s adaptability for single crowns, anterior bridges, and posterior bridges.