Short-span fixed dental prosthesis over omni abutments on the maxillary arch
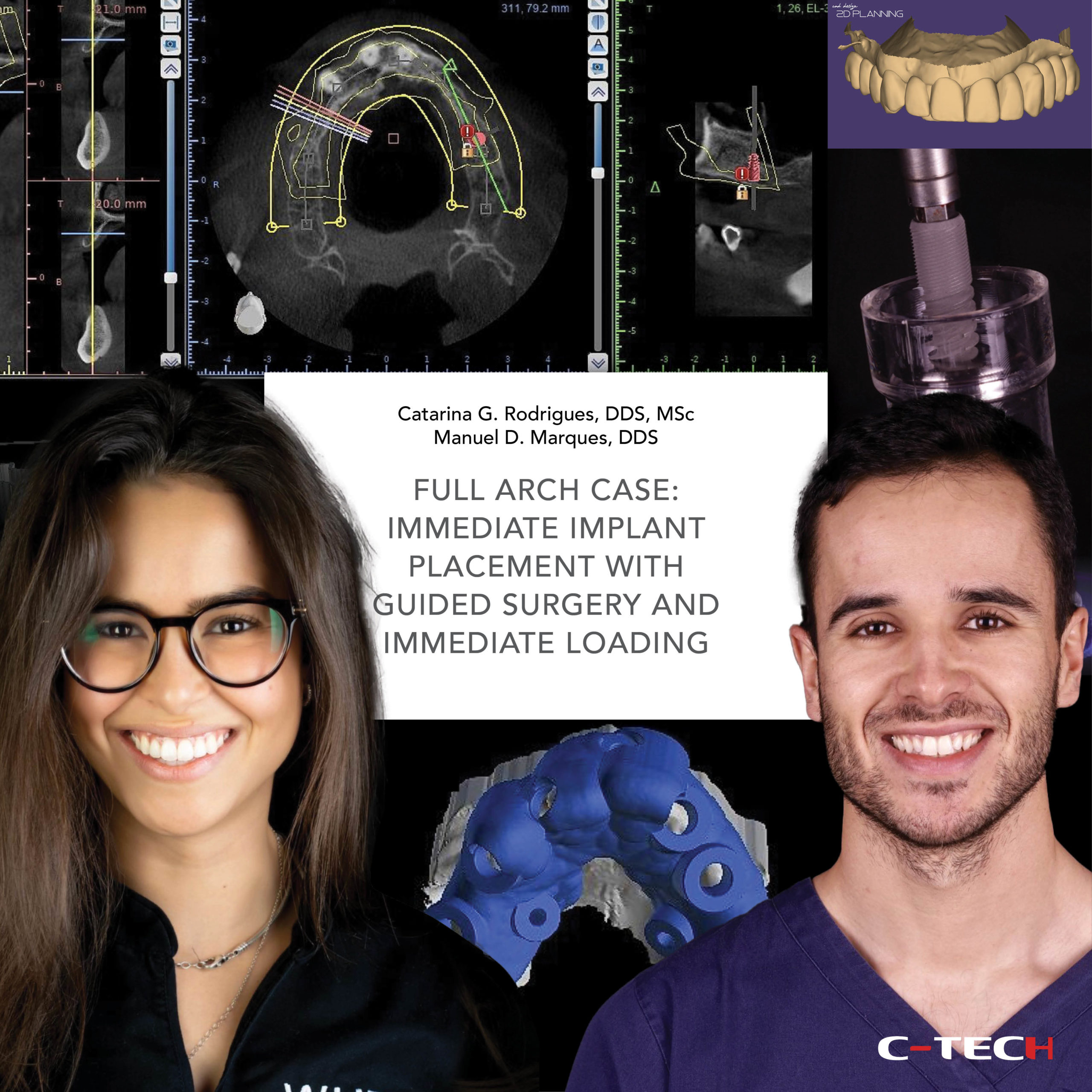
Dr. Catarina G. Rodrigues, DDS, MSc – Dr. Manuel D. Marques, DDS
A 67-year-old woman presented to a private practice reporting discomfort when eating, tooth mobility, and she was unsatisfied with the appearance of her smile. The intraoral and radiographic examination revealed partially edentulous arches, several gingival recessions and carious lesions. Also, a previously failed bone augmentation on the 2nd quadrant as perceived by the scars on the palate (Fig.1). The extra-oral photographs revealed very compromised aesthetic (Fig.2). The initial panoramic x-ray confirmed the significant attachment loss in most of her teeth, especially severe on the upper ones (Fig.3).
Following a comprehensive diagnosis, it was decided to extract all upper teeth and the hopeless teeth on the lower arch. The remaining teeth were maintained and treated by non-surgical mechanical debridement. Then, on the upper arch, it was planned to place 7 dental implants, OMNI abutments and a complete zirconia fixed prosthesis. Immediate loading was also planned for this case. As for the lower, it was planned a short-term orthodontic treatment with invisible aligners to improve tooth position, placement of two implants to replace teeth 44 and 45, and crowns over teeth on the incisors (Fig.4).
In order to perform a proper pre-surgical planning of the case, initial records of the patient were obtained: intra and extra-oral photographs, digital impressions, and CBCT. A 2D facially driven digital smile design was made to aid in the planning of the position and dimension of the teeth for the future interim prosthesis (Fig.5,6).
Then, using a specific 3D CAD software, a digital diagnostic wax-up was generated and 3D printed. A silicone index was obtained from the 3D printed model and filled with bis-acryl resin to produce trial restorations and evaluate the 2D smile planning on the patient’s mouth (Fig.7-9).
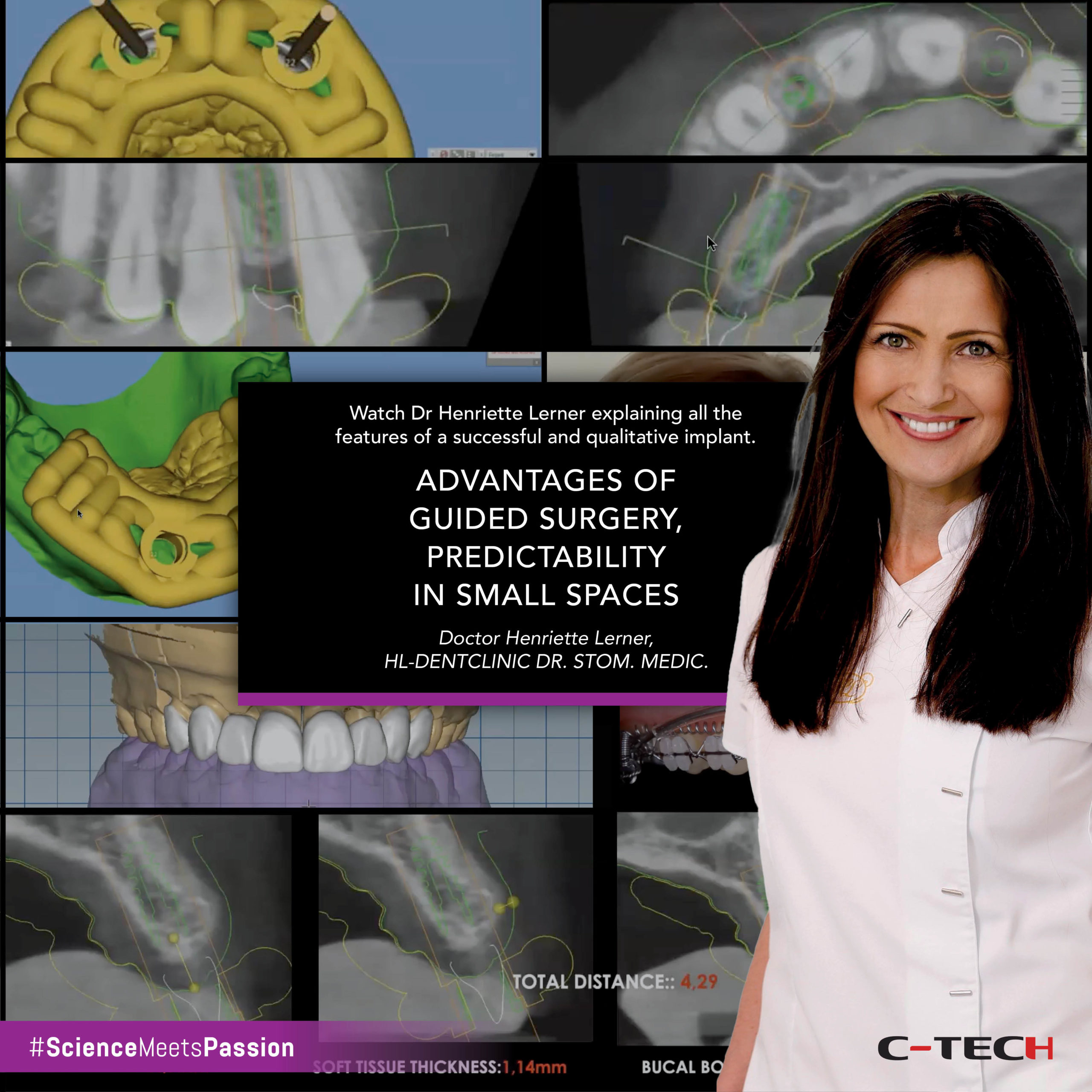
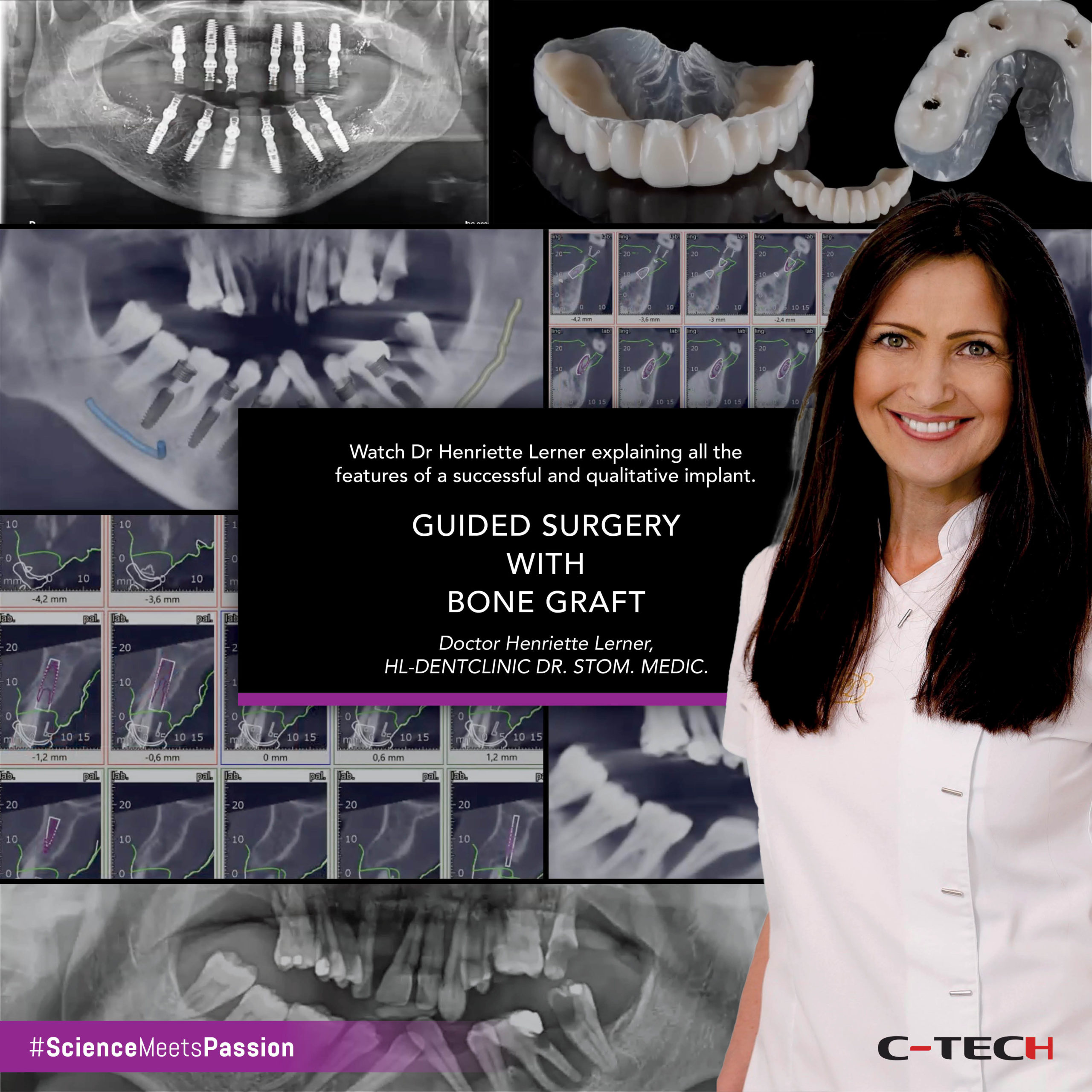
The approved try-in was then scanned and superimposed with the preoperative intra-oral scan and CBCT to digitally plan the implant surgery (Fig.10-12).
Once the future implant positions were defined, they were translated into the design of the surgical guide (Fig.13). The interim prosthesis was also designed and milled from a PMMA disk before the surgery, according to the previously approved mock-up (Fig.14).
The surgical procedure started with the extractions of the hopeless maxillary teeth, very carefully, to preserve the hard and soft tissues as much as possible (Fig.15).
In an occlusal view after the extractions, it is visible that the post-extraction sockets were well preserved. Also, that the molars were left temporarily to give more stability for the surgical guide. (Fig.16).
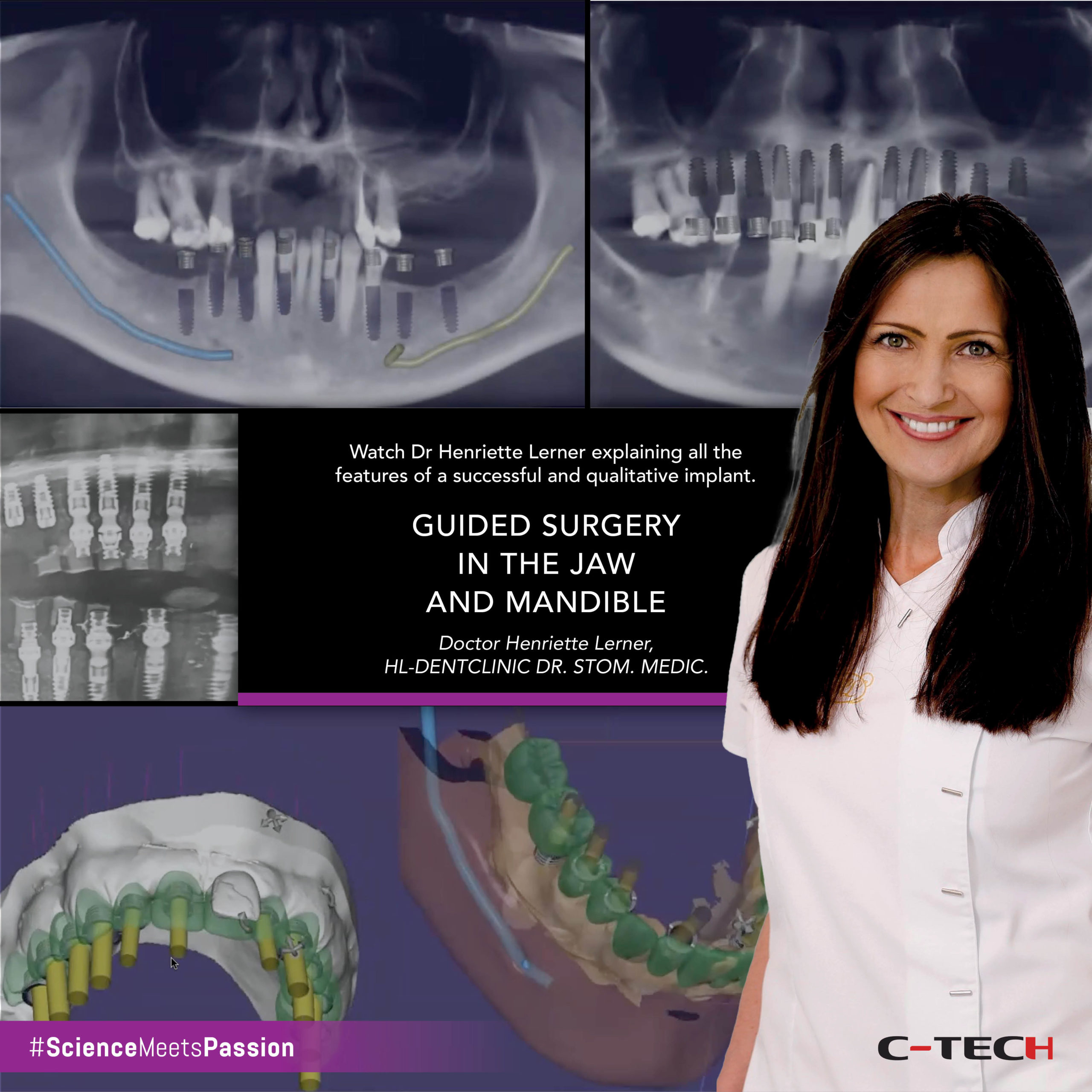
Then, the surgical guide was placed, and the implant sites were prepared through the guide according to a specific drilling protocol, and using C-Tech guided surgery kit, followed by implant placement (Fig.17-19).
After implant placement, OMNI abutments were inserted and torqued in place with 25 Ncm. A full arch provisional screw restoration was delivered the same day (Fig.20-22). However, only five out of the seven implants placed were loaded as the most posterior implant on each side did not achieve enough primary stability to load. The post-operative panoramic x-ray revealed proper fit of the immediate prosthesis to the OMNI abutments (Fig. 23).
One week after the surgery, on the follow-up appointment, we could observe a good healing of the tissues around the provisional prosthesis. Also, the extra-oral pictures one week after the surgery, revealed an improvement of the aesthetics of the patient’s smile (Fig.24,25). Later, on the two-week follow-up surgery, the healing was still progressing well (Fig. 26).
The second stage surgery of the implants that were left submerged occurred 3 months after the implant placement. Also, the OMNI abutments and the corresponding healing caps were placed at this time (Fig. 27).
At this point, the patient informed that she was going to be out of the country for the next two months, so instead of starting the clinical steps to obtain the final restorations, it was decided to ask the lab to produce a new provisional restoration with some modifications in tooth shape, and, especially on the emergence profile, to already start working on gum modulation and prepare everything for the final impressions. The new provisional restoration was delivered, and periapical x-rays were taken to confirm its proper fit (Fig. 28-32).
Finally, 5 months after the implant surgery, and two months after delivering the new provisional restoration, we could proceed with the final impressions. However, after a careful clinical and radiographic evaluation it was come to conclusion that, unfortunately, the implants on 1.6 and 2.6 failed to integrate (Fig.33).
It is well documented in the literature three different types of implant failure: immediate, early and late. In this case, we had an early failure, as it occurred within the first months of implant placement and before placement of the final prosthesis. This type of implant failure is described as solely a biologic complication. In this specific case we could identify the following risk factors: implants placed on the posterior maxilla, D4 type of bone, history of periodontal problems, patient presenting several systemic conditions and polymedicated (Fig.34).
Following the previously described clinical situation, we could go on with two very different approaches which we explained to the patient very carefully. The option one was, to undergo a bone augmentation surgery in each quadrant, then wait at least six months for the healing. After that, another surgery to place the implants and wait three more months for the healing, before we could proceed with final impressions. This was considered the high-risk option, also with a high cost involved and meaning the patient was going to spend at least more 10 to 12 months in treatment.
On the other hand, the option two, was staying only with the five healthy implants she already had and design a short-span fixed dental prosthesis with ten teeth. This one, being the low-risk option, and meaning that in about one month she could have the final prosthesis. Also, it is important to mention that regarding the 1st option, there was the risk of bone augmentation failure, in fact, as previously said, she had already a history of a failed bone augmentation. And also, the risk of implant failure, as this was a high-risk patient for implants. This is to say that she might, nonetheless, must end up with the short-span dental prosthesis (Fig.35).

The short-span fixed dental prosthesis is described in the literature as a treatment strategy that meet the requirements of a functional dentition and does not impair masticatory ability. Also, it is considered to be beneficial for the high-risk patient as it may avoid the risk of overtreatment while still providing a high standard care (Fig.36).
Following all the information provided to the patient, she finally decided for option two. In this case, a complete digital workflow was followed. So, in order to perform the final impressions, the scan abutments were attached to the OMNI (Fig.37-39).
Also, a digital impression of the provisional prosthesis of the patient was obtained to copy important references for the fabrication of the final prosthesis (Fig.40).
 The final prosthesis was produced with a metal framework and zirconia (Fig.41,42).
The final prosthesis was produced with a metal framework and zirconia (Fig.41,42).
In the final intra-oral pictures, we could observe a good integration of the prosthesis with the soft tissues, and with the lower teeth, producing a very natural result. The final periapical x-rays confirmed the proper fit of the final restoration over the OMNI abutments (Fig. 43-45). Also, in the extra-oral pictures, we could appreciate that the reduced number of teeth do not compromise the aesthetics of her smile (Fig. 46,47).
Bibliography
Do, T. A., Le, H. S., Shen, Y. W., Huang, H. L., & Fuh, L. J. (2020). Risk Factors related to Late Failure of Dental Implant-A Systematic Review of Recent Studies. International journal of environmental research and public health, 17(11), 3931.
Mohajerani, H., Roozbayani, R., Taherian, S., & Tabrizi, R. (2017). The Risk Factors in Early Failure of Dental Implants: a Retrospective Study. Journal of dentistry (Shiraz, Iran), 18(4), 298–303.
Yari A., Fasih P., Alborzi S., Nikzad H., & Romoozi E. (2024). Risk factors associated with early implant failure: A retrospective review. Journal of Stomatology, Oral and Maxillofacial Surgery, 125(4), 101749.
Armellini, D., & von Fraunhofer, J. A. (2004). The shortened dental arch: a review of the literature. The Journal of prosthetic dentistry, 92(6), 531–535.
Manola, M., Hussain, F., & Millar, B. J. (2017). Is the shortened dental arch still a satisfactory option?. British dental journal, 223(2), 108–112.
Fueki, K., & Baba, K. (2017). Shortened dental arch and prosthetic effect on oral health-related quality of life: a systematic review and meta-analysis. Journal of oral rehabilitation, 44(7), 563–572.
Witter, D. J., van Palenstein Helderman, W. H., Creugers, N. H., & Käyser, A. F. (1999). The shortened dental arch concept and its implications for oral health care. Community dentistry and oral epidemiology, 27(4), 249–258.
Webinar | OMNI AESTHETIC SOLUTIONS: from single units to full arch
Catarina G. Rodrigues, DDS, MSc • Manuel D. Marques, DDS
This webinar introduces the OMNI abutment by C-Tech, a versatile prosthetic component designed to achieve excellent aesthetic results across various dental cases, from single units to full arches. The presentation begins with a complex full-mouth case demonstrating the OMNI abutment’s adaptability for single crowns, anterior bridges, and posterior bridges.