Rehabilitation of atrophic maxilla combining GBR and dental implants
Dr. Santiago Fernández Sánchez (Dentist: surgical and restorative procedure) Technician: Simón Lamela
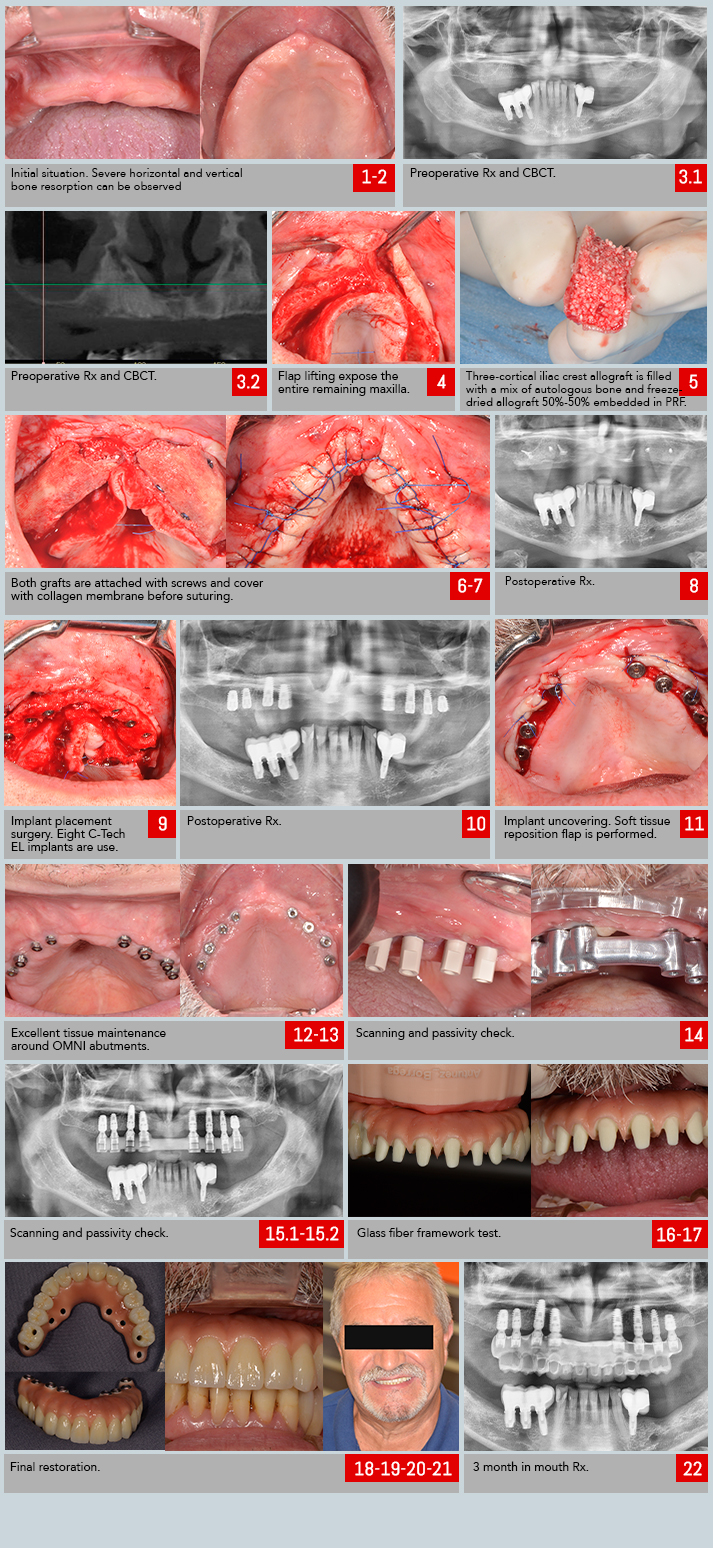
The patient, a male 64 years old, no significant medical condition or smoker; had a long term complete edentulous condition on the upper jaw, more than 15 years (fig. 1 & 2).
In this time, he visited several professionals without finding any solution other than removal prosthesis due to the extreme resorption of his remanent bone. After exploring the case in addition to CBCT and Rx (fig. 3.1 & 3.2) we considered to offering the patient the following solution: fixed restoration supported by 8 implants, placed after a GBR procedure.
We considered the no smoking condition crucial for the success of the regenerative procedure, due to the limited osteogenic surface we had at our disposal.
For this case we used freeze-dried human bone offered by a local tissue bank. A three-cortical iliac crest piece was selected, big enough to cover both sides of the maxilla. During the surgery, a wide flap was raised in order to uncover the entire remaining bone (fig. 4).
After that, all the cancellous bone was cleared out from the graft so it could be filled with a mix of autologous bone and freeze-dried allograft in a 50/50 proportion (fig. 5).
Patients bone was collected by scratching from the same surgical area, specially from pyramidal apophysis of the zygoma. The mixture was soaked in PRF, improving the angiogenesis inside the graft once placed in site. Both grafts were fixed using screws (fig. 6) and covered with collagen membrane intended to work as a barrier against soft tissue for at least 16 weeks (fig. 7 & 8).
Implant surgery took place after 16 weeks of healing time: 8 C-Tech EL implants were placed after removing the screws that remained from the previous surgery. We could now work in a wider bone crest that allowed us to avoid the use of narrow diameter implants.
As the sinus were highly pneumatized, sinus floor rise was performed in both of them using densification drilling protocol. (fig 9 & 10).
We also performed a relining graft using freeze-dried allograft trying to get a regular shape with smooth surface. As well as in the first surgery, the graft was covered with a collagen membrane. All parameters measured along the surgery suggested that waiting other 16 weeks for the tissues to heal would be enough.
A removal prosthesis was used by the patient as temporary restoration during all the process. Once that time passed, we uncovered the implants by repositioning soft tissue buccally (fig. 11).
Conventional healing abutments were used until suture was removed and then replaced by OMNI straight abutments. We chose these abutments due to their reduced diameter and strong prosthetic screw but also for its excellent soft tissue treatment, improving patients cleaning capacity (fig. 11 & 12).
We started then the prosthetic procedure, digitally scanning the scanbodies of the system (fig. 13 & 14).
The technician sent us the first framework to be checked: a milled aluminum structure used to verify passivity and replace – if needed – the position of any of the implants on the printed model (fig. 15.1 & 15.2). In our case, no changes were required and we went straight to the next step: Aesthetics.
As we needed to recover a big volume with this restoration – that involved teeth, soft and hard tissue – we decided to make a glass fiber framework. That option allowed us to considerably reduce final weight of the prosthesis while a different restoration material can be chosen depending on requirements of each tooth.
We made the decision to individualize teeth from 14 to 24 cementing individual Emax ceramic crowns to the glass fiber base, previously designed for that objective. That would improve the aesthetic of the restoration. For second bicuspids and first molars, we decided to apply composite directly on the glass fiber base for functional reasons.
Posterior area of the patients lower jaw was rehabilitated with dental implants before we met. We preferred not to restore our implants with rigid solutions when they’re facing implants with similar solutions. Glass fiber framework combined with composite will offer a more resilient behavior and a more pleasant feeling to the patient when occluding with the antagonist. Aesthetic gum was also made in composite (fig. 16).
Finally, restoration was finished and screwed in its final position (fig. 18-22). Further treatment will be needed on the lower jaw implants.