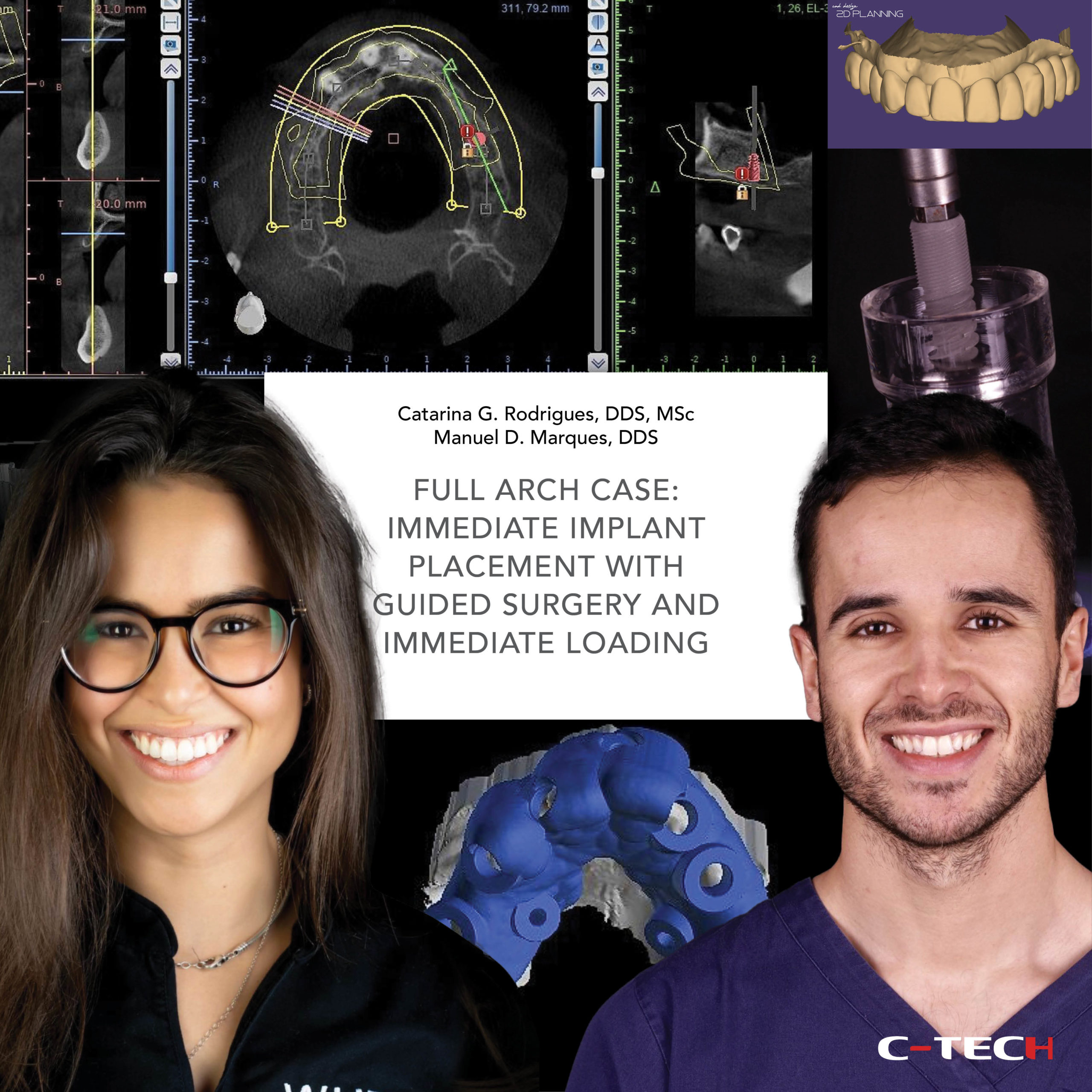
Full arch rehabilitation combining guided surgery and socket shield technique with immediate loading
Dr. Santiago Fernández Sánchez (Dentist: surgical and restorative procedure) Dental Technician: Simón Lamela
Patient: 71-years-old woman. Medically controlled Arterial Hypertension. Unpleased with how she looks when smile and no comfortable due to teeth movement. Presents advanced periodontal disease with and average bone loss over 50% in upper maxilla, which lead to type II mobility on several teeth. Lower jaw was less affected (average bone loss around 30%) despite teeth 47 and 37 were to be extracted.
Periodontal treatment followed by fixed prosthetic restoration supported by her teeth was rejected by the patient, who was “tired of her teeth”.(Fig. 1-4)
 Then we proposed periodontal treatment to improve biological condition and reduce teeth mobility to perform the socket preservation technique called Socket Shield Technique. This technique offers optimal tissue maintenance by leaving a fragment of the root (shield) attached to the buccal plate of the socket during extraction. This root fragment keeps periodontal system working over the external surface of the root, including the vascular complex that provides blood support to the buccal bone plate. Absence of root mobility is essential.
Then we proposed periodontal treatment to improve biological condition and reduce teeth mobility to perform the socket preservation technique called Socket Shield Technique. This technique offers optimal tissue maintenance by leaving a fragment of the root (shield) attached to the buccal plate of the socket during extraction. This root fragment keeps periodontal system working over the external surface of the root, including the vascular complex that provides blood support to the buccal bone plate. Absence of root mobility is essential.
Once the periodontal treatment objectives were achieved, eight implant planning over a CBCT was done and a surgical guide was made, as well as a provisional prosthesis.
Surgery started with the extraction of teeth on where implants were going to be place. (Fig. 5)
Socket Shield Technique was performed on every tooth extracted, even on those sockets on where no implant was programmed in order to get the best tissue maintenance. Remanent teeth worked as support for the surgical guide. (Fig. 6,7)
 After guided implant placement, the rest of teeth were extracted (Fig. 8). Implant insertion torque was over 35N. Eight straight MUA abutments were used (Fig. 9) before filling those sockets without implants with a mixture of alloplastic hydroxyapatite and PRF. (Fig. 10)
After guided implant placement, the rest of teeth were extracted (Fig. 8). Implant insertion torque was over 35N. Eight straight MUA abutments were used (Fig. 9) before filling those sockets without implants with a mixture of alloplastic hydroxyapatite and PRF. (Fig. 10)
 Only PRF was place around implants. Provisional prosthesis was screwed in position after suturing the only place a little flap was rised. (Fig. 11)
Only PRF was place around implants. Provisional prosthesis was screwed in position after suturing the only place a little flap was rised. (Fig. 11)
Extraction of 37 and 47 were done and implants in position 45, 46 and 36 were placed. Three days after surgery, the patient confirmed the excellent outcome of the surgery, with absolute absence of swelling, pain or bleeding. (Fig.12-15)
Four months on, we started with definitive restoration procedure by scanning the MUA abutments and subsequently checking passivity. (Fig.16-18).
 At this time we can observe that the healing process had no cost in terms of tissue remodeling or volume loss. (Fig.19-21)
At this time we can observe that the healing process had no cost in terms of tissue remodeling or volume loss. (Fig.19-21)
 This is especially evident when comparing tissue condition before surgery with present.
This is especially evident when comparing tissue condition before surgery with present.
Finally, we fixed the zirconia-porcelain restoration on its definitive position, giving the patient the highly desired smile. (Fig.22-25)
 Looking at the control X-Ray (26), done 8 months after the final restoration, we can appreciate bone level holding not only around implants connection but millimeters away from there, resting over the abutments. That behavior can be observed around every single implant, showing how a Cone Morse connection influences the biology of peri implant tissues.
Looking at the control X-Ray (26), done 8 months after the final restoration, we can appreciate bone level holding not only around implants connection but millimeters away from there, resting over the abutments. That behavior can be observed around every single implant, showing how a Cone Morse connection influences the biology of peri implant tissues.
Combination of Socket Shield Technique and Cone Morse connection may represent an significant difference in hard and soft tissue maintenance.